1
Brand-Name vs. Generic Drugs: What Patients Really Need to Know

You ever get the pharmacy bill and feel like you’re being charged for a small diamond instead of a bottle of pills? Then the pharmacist points to the generic version and promises it will fix your wallet—no fancy label, just the same active ingredients. Still, something makes you wonder: is the generic really as good as the brand-name? There’s a lot of noise out there. Some folks swear by their faithful brand-name meds, while others say generics are a no-brainer. To get past the marketing haze, let’s dive into how these drugs end up on the shelf, what truly sets them apart, and when it matters most for your health and your cash.
What Are Brand-Name and Generic Drugs, Anyway?
Brand-name drugs are the originals—the ones with the catchy ads, memorable colors, and big pharma logos. They’re developed from scratch, often discovered after years of research and hundreds of millions (sometimes billions) of dollars. Once a pharmaceutical company invents and tests a new drug, it gets a patent, usually lasting 20 years from when they first apply for it—though the clock starts ticking way before the drug appears on shelves. This patent means their competition can’t sell the same active medicine as a generic, giving the brand a virtual monopoly.
Generics step onto the stage a bit later. Once the brand-name patent expires, other drug makers can offer their versions—called generics. Here’s what matters: generics have to prove to the FDA that their product has the same active ingredient, strength, dosage form (like pill or liquid), and method of use as the brand drug. But they skip all the expensive discovery steps, so their costs to produce are lower. Roughly 9 out of 10 prescriptions filled in the U.S. today are for generics, according to the FDA in a report from late 2024.
What’s really different? Packaging, price, and sometimes those non-active ingredients known as fillers or binders (think dyes or flavor coatings). And, frankly, the trust factor—some patients just feel more at ease with the brand name they’ve seen advertised or have used for years. But the FDA requires every generic to deliver the same "bioequivalence"—it has to work in your body in the same way and time as the original.
Consider this: there are over 10,000 FDA-approved generic drugs, and for each one, there’s a stack of paperwork showing it meets strict criteria. The cost savings aren’t small beer either. According to a study from Johns Hopkins published in March 2025, patients and insurers in the U.S. saved over $373 billion in 2023 by choosing generics over brand names. That’s a lot of college tuition, vacation money, or emergency savings—just from switching pill bottles.
Testing and Approval: Is There Really a Difference?
This is where things get interesting. When a brand drug is first invented, the manufacturer has to put it through intense trials: making sure it actually works for people and doesn’t cause too many dangerous side effects. We’re talking about thousands of people, years of work, and enormous investment. These are called "clinical trials," and getting a drug through them is a massive undertaking.
Once a generic wants to join the party, the rules change. Since the brand drug already showed that the ingredient works, generics just need to prove their version matches the original in key ways. The main gold standard here is something called "bioequivalence." Basically, they have to show that if you take the same dose of generic, it delivers the same amount of medicine into your bloodstream at about the same speed as the brand. They test this with healthy volunteers—usually just a few dozen people, not the thousands used for the brand drug’s original approval.
Some folks might get nervous here. Doesn't that mean generics are less tested? Not quite. Every single generic batch is tightly regulated by the FDA—down to surprise plant inspections and regular quality checks. In fact, a big 2023 Government Accountability Office (GAO) report found that generic drug manufacturing plants had a similar or even better track record for FDA compliance than brand-name plants.
Still, there are a couple of exceptions to the usual rules. Sometimes, the inactive ingredients in generics can affect how the body absorbs the drug. For a tiny group of drugs—known as “narrow therapeutic index” medicines—small changes in blood levels can mean the difference between working and not working, or even causing harm. Examples include seizure meds like phenytoin or anti-rejection drugs for transplants. If you’re taking one of these, most doctors and pharmacists suggest sticking with either the brand-name or a consistent generic manufacturer rather than jumping brands.
Let’s look at how things stack up:
| Feature | Brand-Name Drug | Generic Drug |
|---|---|---|
| Active Ingredient | Original, patented formula | Exactly the same |
| Inactive Ingredients | Standard set | Can vary (colors, preservatives, fillers) |
| Clinical Trial Size | Thousands of patients | Dozens of healthy volunteers (bioequivalence) |
| FDA Supervision | Yes | Yes |
| Cost | Average: $300-500/month | Average: $10-40/month |
| Effectiveness | Proven safe & effective | Proven bioequivalent |
Money Talks: The Shocking Cost Gap Between Brand-Name and Generic Drugs
The sticker shock at the pharmacy is the number one reason people even ask about generics. Here’s the straight talk: as soon as a drug loses its patent, competitors swoop in, making prices nosedive. The price tag for a generic can be 80–85% lower than its brand-name cousin. The FDA keeps a running list, and in 2024, generic amlodipine for high blood pressure averaged about $8 for a month’s supply, while the branded version, Norvasc, costs closer to $150—not counting insurance.
Why this dramatic drop? Generic makers don’t have to bankroll the original research or years of advertising. Once they prove their product matches the brand in performance and safety, it’s mass production time. And with more than one generic supplier gunning for a piece of the pie, competition keeps prices brutally low.
Let’s get specific. According to a study released by the Association for Accessible Medicines in 2025, an average American family saves nearly $1,500 per year just by choosing generics over brands for ongoing prescriptions. That sort of saving can mean deciding between putting gas in the car or skipping a necessary refill. And since nearly half of Americans take at least one prescription medicine, the impact stretches across millions of people and their families every year.
Insurance, of course, plays a starring role. Most plans greatly prefer generics. Your insurer might even flat-out deny coverage for the brand unless the doctor writes 'dispense as written.' Even then, you could be left paying most of the bill. Medicare and Medicaid have stacked their formularies with generics to keep costs low for both patients and taxpayers.
But here’s a hot tip: always ask if there’s a generic option for your prescription or over-the-counter (OTC) meds. Doctors might default to writing for the brand just out of habit or because of recent pharmaceutical sales visits. Pharmacists are your secret weapon—they can usually substitute a generic unless your prescriber says otherwise. If you’re nervous about the switch, ask your pharmacist if the same manufacturer’s generic is always stocked, so you don’t bounce between different versions every time you refill.
When It Matters: Picking the Right Drug for You
So, does choosing a generic really work for everyone? For the overwhelming majority, the answer is yes. The brand-name drugs might have a fancier logo and slicker packaging, but if you read the fine print, you’ll see that the FDA holds both sides to the same set of high standards for safety and effectiveness. Most people can’t tell a difference in how they feel or how their health measures look after switching from brand to generic.
But there’s a reason you meet a few people who insist the brand works better for them. Sometimes, it’s about the inactive ingredients. Some folks have allergies or intolerances to food dyes, stabilizers, or preservatives used in generics but not in the brand—though this is pretty rare. And those narrow therapeutic index drugs? If you’re on meds like warfarin (a blood thinner) or levothyroxine (thyroid replacement), keep careful notes if you switch, and always let your doctor know. Blood tests after a switch can check if your dosage is still right.
If you or your kid have trouble swallowing certain large generic pills, ask the pharmacy for alternative generic brands (they can vary in shape, size, or coatings). Many companies even offer scored tablets, liquid versions, or melt-in-your-mouth forms, at the same low generic price.
How about for mental health meds? For a tiny slice of patients on antidepressants or antipsychotics, the switch to a generic can feel different—sometimes because of how the body absorbs the drug, sometimes just from expectation. If you notice a big shift in symptoms after a switch, bring it up immediately with your doctor. Just don’t stop the new pill cold turkey before talking it out—you might experience withdrawal or a return of tough symptoms.
Traveling abroad or shopping at online pharmacies? Watch out. The strict standards we rely on in the U.S. aren’t as consistent everywhere else. If you’re buying medicine from another country or an unknown online seller, you might run into capsules that don’t actually contain what the label says. Always stick to legitimate, licensed pharmacies. If you’re saving a ton by going international, do some digging to be absolutely sure they’re registered and approved.
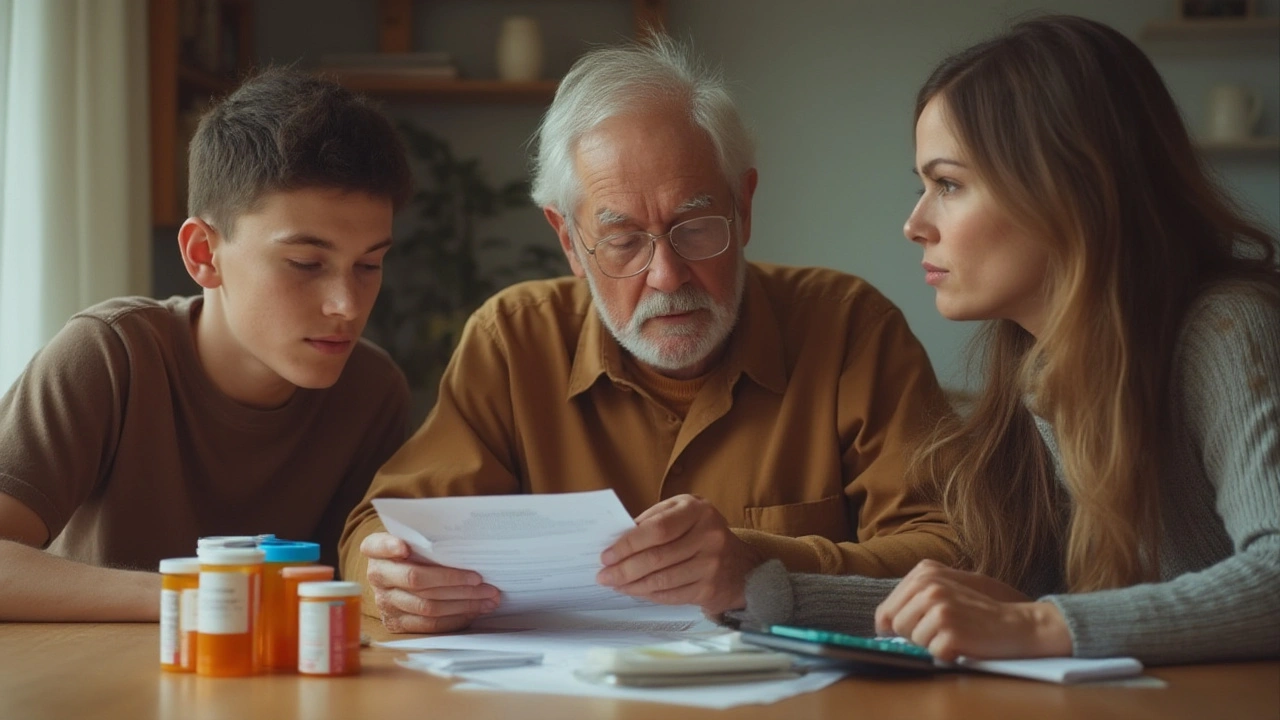
One final tip: for medicine cabinets with several generics (especially stuff like blood pressure meds), use a pill organizer or label your bottles clearly. Some generics change in color or shape from refill to refill, since different suppliers get cycled in. This can be confusing for anyone keeping track of more than one daily pill, especially seniors or those helping out an older family member.
If you’re worried about switching from brand to generic, don’t go it alone. Pharmacists love talking shop. They’re often easier to reach than your doctor, and they know the ins and outs of how each version works. And if cost is holding you back from the medicine your doctor prescribed, don’t just let your prescription collect dust—ask about patient assistance programs or check GoodRx for discount coupons. There’s nearly always a way to get what you need without emptying your wallet.