Support: Understanding Antibiotic Resistance and Keeping Your Health Safe
Antibiotic resistance is more than just a medical term—it’s a reality that could affect you or someone you care about. When bacteria become resistant to antibiotics, the medicines we rely on stop working, which makes infections harder to treat. This page is here to give you clear, straightforward info about what causes antibiotic resistance and what you can do to stay safe.
What Causes Antibiotic Resistance?
You might wonder why bacteria become resistant in the first place. It happens mostly because antibiotics are used too much or incorrectly. For example, if someone stops taking their antibiotics too early or uses them for a viral infection like a cold, the bacteria can learn to fight back. Resistant bacteria then multiply, making superbugs that resist many treatments.
This isn’t just a problem for hospitals or sick people—it affects everyone. Resistant infections can spread in communities and even in everyday settings like schools or workplaces, so understanding this helps you act wisely.
How Can You Protect Yourself and Others?
The good news? There are practical steps you can take every day. First, only use antibiotics when prescribed by a healthcare professional. Don’t insist on them if your doctor says you don’t need them. Finish the full course even if you feel better, so no bacteria get the chance to survive and adapt.
Keeping good hygiene, like washing hands regularly, also helps stop the spread of bacteria. And remember, vaccinations can prevent certain infections, reducing the need for antibiotics in the first place.
Looking out for these simple actions helps you protect your health and slows down antibiotic resistance, benefiting the whole community.
18
Prime Video on Roku, Fire TV, Apple TV, and Smart TVs: Step-by-Step Setup Guide
Learn how to set up Prime Video on Roku, Fire TV, Apple TV, and smart TVs with step-by-step instructions. Fix common errors, check streaming quality, and manage profiles easily.
9
Accessibility Settings for Streaming: Captions, Audio Descriptions, and Remotes
Learn how to set up captions, audio descriptions, and accessible remotes for streaming services to make TV and movies easier to enjoy for people with hearing, vision, or mobility challenges. Simple fixes can transform your viewing experience.
24
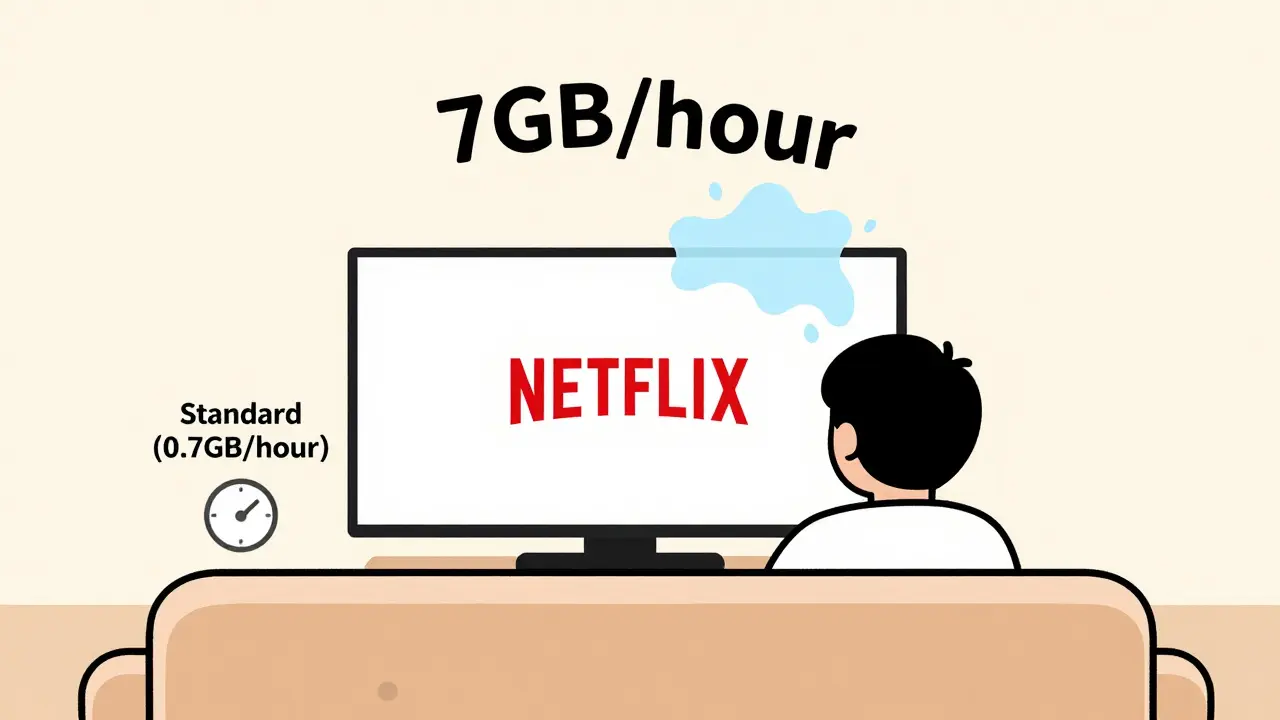
Data Caps and Streaming: How Much Data Does Streaming Use?
Learn how much data streaming services like Netflix, YouTube, and Disney+ use per hour, how to track your usage, and simple ways to cut data without losing quality-especially if you're on a limited plan.
22
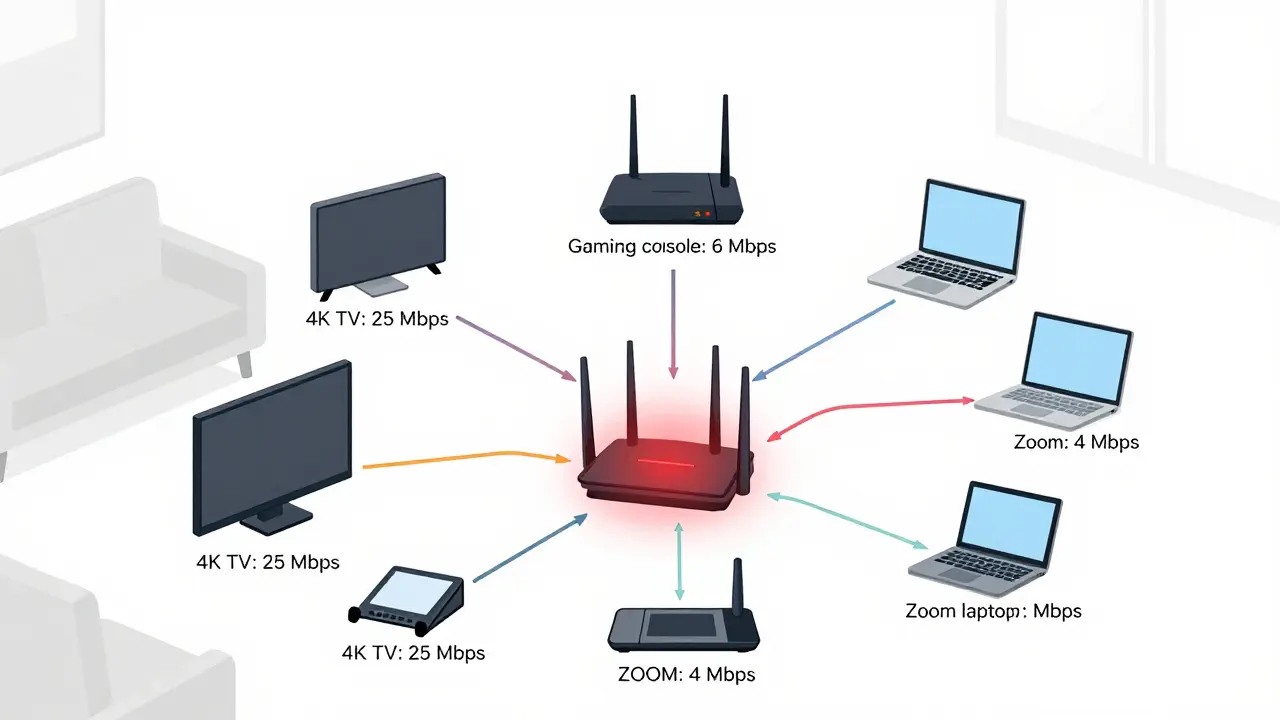
How to Allocate Bandwidth for Multiple Streaming Devices Without Buffering
Learn how to allocate bandwidth for multiple streaming devices to avoid buffering. Get practical tips on router settings, internet plans, and QoS to keep all your streams running smoothly.
15
Roku Remote Finder and Rechargeable Remotes: Which Models Include Them
Learn which Roku models include a remote finder and rechargeable battery to stop losing your remote and wasting money on batteries. Find the right upgrade without buying a new player.
14
Switching Streaming Tiers Mid-Cycle: How Billing Adjustments Work
Learn how streaming services adjust your bill when you upgrade or downgrade mid-cycle. No overcharges. No surprises. Just fair, prorated pricing based on what you actually used.
3
How to Reduce Netflix Data Usage Without Losing Video Quality
Learn how to reduce Netflix data usage without losing video quality. Simple settings changes can cut your data use by up to 70%, helping you stay under your monthly cap.
29
Live Stream Safety: How to Avoid Bans and Stay Within Platform Policies
Learn how to avoid live stream bans by understanding platform policies, recognizing gray-area violations, and using moderation tools to keep your channel safe and active.
27
Billing and Payment Lockouts: How to Restore Streaming Access Fast
Fix a billing lockout on your streaming service fast with these simple steps. Learn why payment failures happen and how to restore access without calling support.
19
How to Expand Storage on Fire TV with USB Drives and Manage Apps Better
Learn how to expand storage on your Fire TV using USB drives and manage apps to stop storage warnings. Clear cache, move compatible apps, and extend your device's life without buying new hardware.
8
How Roommates Can Fairly Share Wi-Fi and Streaming Costs
Learn how to fairly split Wi-Fi and streaming costs with roommates to avoid conflict, save money, and keep relationships smooth. Simple, practical system for 2025.
3
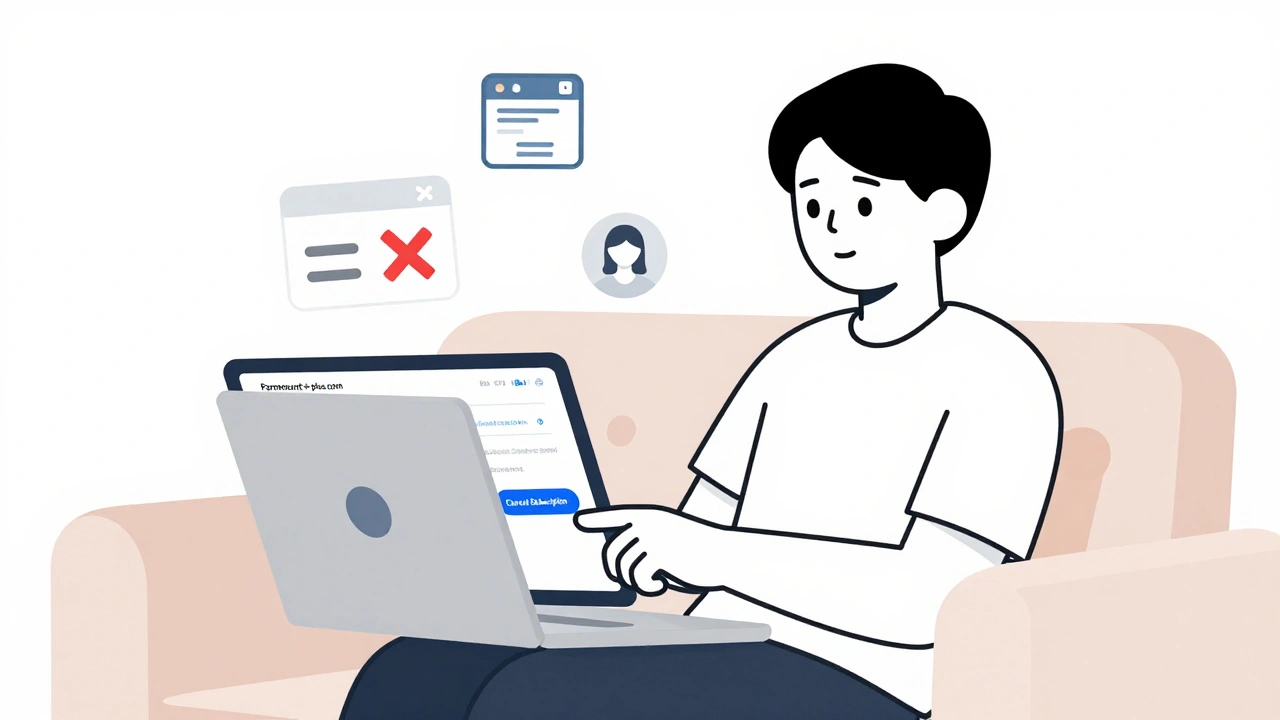
How to Cancel Paramount+: Step-by-Step Guide
Learn how to cancel Paramount+ on any device - web, iPhone, Android, Roku, or Smart TV. Avoid hidden charges, keep your watch history, and know what happens after cancellation.
Latest Posts
Popular Posts
-
 Netflix Recommended Internet Speeds: Official Requirements Explained
Netflix Recommended Internet Speeds: Official Requirements Explained
-
 Prime Video on Roku, Fire TV, Apple TV, and Smart TVs: Step-by-Step Setup Guide
Prime Video on Roku, Fire TV, Apple TV, and Smart TVs: Step-by-Step Setup Guide
-
 Accessibility Settings for Streaming: Captions, Audio Descriptions, and Remotes
Accessibility Settings for Streaming: Captions, Audio Descriptions, and Remotes
-
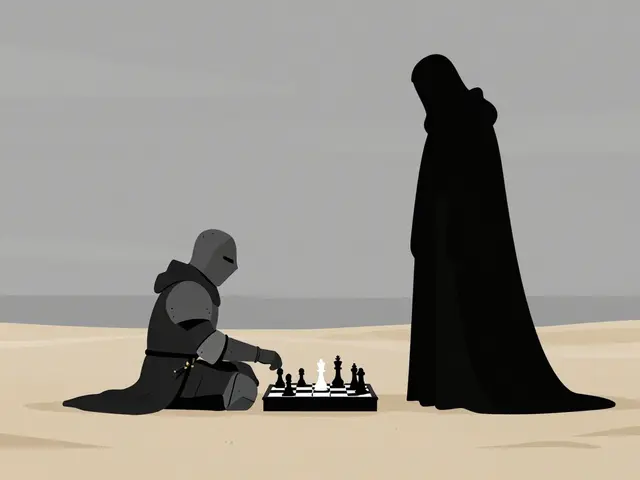 The Seventh Seal Explained: Ingmar Bergman’s Medieval Meditation on Death
The Seventh Seal Explained: Ingmar Bergman’s Medieval Meditation on Death
-
 Max Parental Controls: Create Kid Profiles and Set Content Ratings
Max Parental Controls: Create Kid Profiles and Set Content Ratings
Categories
Tags
- streaming services
- video editing
- video production
- parental controls
- Max streaming
- video editing software
- marketing mix
- subscription management
- streaming apps
- video editing tips
- tips
- ROI
- video marketing
- video editing tools
- marketing strategy
- Premiere Pro
- family viewing
- classic cinema
- Kurosawa
- streaming setup